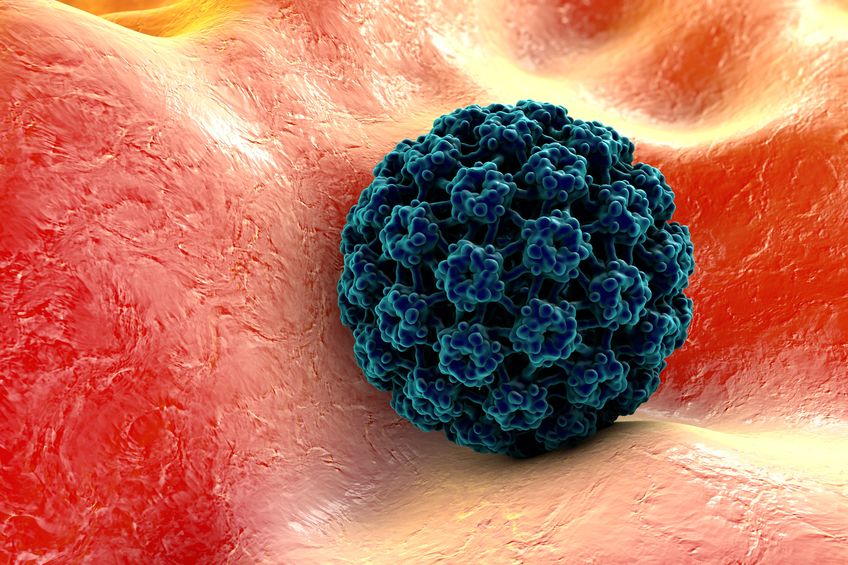
48858475 – background with virus. human papillomavirus on the surface of a cell. a model is built using data of viral macromolecular structure from protein data bank pdb 3j6r
CONDYLOMATA ACUMINATA (ANAL PAPILLOMATA OR WARTS)
Genital papillomavirus (HPV) infections are considered the most common sexually transmitted infection (STI). It is estimated that they affect 30 million women and men worldwide. The United States reports one million new cases each year. The frequency of anogenital condyloma is particularly high in people infected with the AIDS virus (HIV).
About 4% of all cancers are associated with HPV. In the United States, an estimated 32,000 cases of cancer diagnosed in men and women in 2009 were attributable to HPV infection. For several years, we know for sure that this infection is responsible for cancer of the cervix. Oncogenic HPV is involved in at least 80% of anal cancers and 40% to 60% of cancers of the vulva, vagina and penis. They have also been implicated in a subgroup of head and neck cancers.
Definition
Warts arising from the skin of the anal canal and perianal region have been a relatively common occurence since earliest time. Even physicians of ancient Rome were familiar with this condition, which they referred to as ‘figs’. In the past, a relationship to venereal disease has been suspected and the warts were variously ascribed to syphilis, gonorrhoea, and non-specific irritation by dirt and discharges. In the last three decades, however, anal warts seem to have become much more common, in keeping with active male homosexuality and heterosexual anal coitus, with which these tumours are mostly connected.
There are more than 222 different types of HPV. Some are particularly feared, especially HPV 16 and 18, called “high risk” because they are responsab for anal and cervix cancers. They are found, for example, in 90% of anal cancers, 65% of cancers of the cervix and vagina, 50% of vulvar cancers, 35% of penile cancers, and 45% to 90% of cancers.
Other HPVs do not cause cancer but are nonetheless troublesome for their carriers. This is for example the case of HPV 6 and 11 which are said to be “low risk” because they do not cause cancer. They are not trivial since they are responsible for genital warts or genital warts (warts). These HPV 6 and 11 are targeted by Gardasil.
HPV 16 and 18 are targeted by existing vaccines (Cervarix and Gardasil). However, it is important not to extrapolate the proven interest of these vaccines for the anogenital area to bucal manifestation, since it is unclear for lack of study what would be their effectiveness on oral infections.
The mechanisms of malignification is not well understood. For example, it is not known why 10% of people infected with HPV will not be able to eliminate it within two years and become chronic carriers of the virus while the remaining 90% achieve elimination. It is also not known why only half of these chronic carriers will have cancer after about thirty years.
INCIDENCE
Age and Sex.
Anal warts can occur at any time from childhood to old age in either sex. If it was previously far more common in young males than in any other class of patient, female are increasing in incidence in our clinic.
Frequency of Homosexuality. Studies show that 95% of their male patients and 34% of their female patients admitted to having anal coitus;
Associated Genital Warts
A certain number of patients with anal warts also have genital warts more so in women (80%) than men (16%).
Last year, Professor Maura Gillison of the University of Ohio and colleagues in Rockville, Maryland, reported in the Journal of the American Medical Association (JAMA) the prevalence of oral HPV infection in the general population. Americans aged 14 to 59 years: 1.6% of men and 0.3% of women were infected with HPV 16. The risk was even higher when using tobacco, alcohol or cannabis. The gap between men and women, however, is not explained, especially since it persists even after a statistical correction incorporating high risk behaviors, more common in men.
For the authors, there is no doubt that HPV infection is mainly sexually transmitted because the risk of carrying the virus increases proportionally to the number of sexual partners that we have already had. The trivialization of oral sex in couples could well explain the increase of oropharyngeal cancers. In France, 91% of women and 94% of men aged 18 to 69 reported having already practiced oral sex in the last major survey on French sexuality in 2006 (Bajos, Bozon, La Découverte 2008), while they were 51% and 54% respectively in the 1970 national survey.
Recurrent respiratory papillomatosis is a rare disease.
AETIOLOGY
Anal warts are of viral origin; they are a sexually transmitted infection (STI) caused by certain strains of the human papillomavirus (HPV). The incubation period varies from one to six months or even longer. They are especially dangerous for women because some types of HPV can also cause cancer of the cervix and vulva and anal cancer in both sex.
Transmission is usually cutaneous.
Human papillomavirus (HPV) is usually transmitted by direct skin-to-skin contact and, in genital infections, most often, but not exclusively, in penetrative sex.
A small lesion of the skin (scratch) or mucous membranes is enough for the virus to enter the body. Its transmission could also be done indirectly through contaminated objects. Attendance at public places such as swimming pools, gymnasiums, sports clubs … is one of the transmission methods classically mentioned for cutaneous plantar warts.
All sexual practices can be contaminating, including oral intercourse, in heterosexual and homosexual couples. The higher the number of sexual partners, the greater the risk of transmission. Similarly, the existence of another sexually transmitted infection, by damaging the ano-genital mucosa, facilitates contamination. Men have an important role in the transmission of HPV to women.
CLINICAL FEATURES
The human papillomavirus (HPV) family has many different types that cause different diseases.
Some of them cause benign lesions of the skin (warts), mucous membranes of the genital and anal regions (condylomata) or extragenital (papillomas of the mouth) or of the respiratory system (recurrent respiratory papillomatosis) .
These types of papillomavirus, which are mainly HPV 6 and 11, are called low risk.
Other types are responsible for sexually transmitted infections and cancers, mainly that of the cervix.
These are high-risk papillomaviruses, known as oncogenes, the most common of which are HPV 16 and 18.
Vaccines protect against serotypes responsible for about 70% of these cancers. They do not dispense with regular smear checks from 25 years old
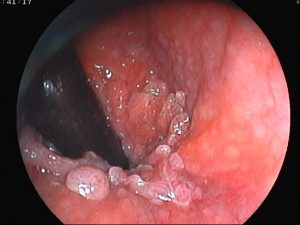
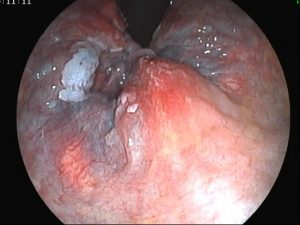
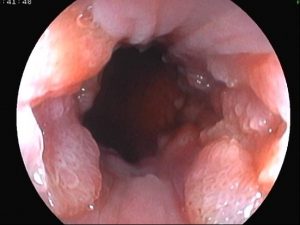
Gross Appearances.
Anal warts may be single, but are nearly always multiple and very numerous. The individual wart may be sessile or pedunculated, a mixture of the two types often being present in the same patient. They vary in size from that of a match-head to 1—2 cm across or bigger. They are initially pink in colour and their surface is usually papilliform, but the warmth and moisture of the anal region often result in their becoming sodden and whitened. Frequently they exude an irritating discharge with a disagreeable odour. The warts tend to be friable, and when rubbed may bleed.
The warts are located not only in the perianal skin but also, in the great majority of patients—actually in in the skin of the anal canal up to the pectinate line. It is very easy to miss these lesions in the canal unless a careful proctoscopic examination is carried out, and this oversight may have considerable therapeutic implications. In female patients extension of the warts to the vulva is also very common.
Symptoms
Though most patients with anal warts are aware of them, they usually have only slight symptoms—some irritation, a certain amount of moisture or discharge in the anal region, occasional bleeding at defaecation or subsequently, and, if the warts are very numerous, difficulty in cleansing the anal region. In women patients the discharge may be thought to be coining from the vagina, as indeed some of it may if there are also warts on the vulva.
Anal verge
DIAGNOSIS
In most cases the diagnosis is easy. But confusion may arise with the condylomata lata of secondary syphilis. However, they are fewer in number, smoother and flatter, and look more like areas of granulation tissue. Other clinical manifestations of secondary syphilis may be present, and the diagnosis can be readily established by having a small quantity of the glairy discharge examined by dark-ground illumination for the spirochaetes which usually are present in large numbers. It should be remembered, of course, that the two forms of condylomata may be present in the same case.
Another condition that may require to be differentiated is a squamous cell carcinoma of the anus; it is more indurated and ulcerated as a rule and a routine biopsy confirms the diagnosis.
In addition to routine digital and endoscopic examination of the anorectum, and examination of the genitalia, one should have a rectal and urethral swab for gonococci, a serological test for syphilis and possibly stool examinations to exclude pathogens.
Anal warts have an unenviable reputation for recurrence after treatment. But it must be emphasized that it has been very difficult to determine exactly how often they recur. The reason is that there is a considerable risk of re-infection from the original infecting partner or some other subsequent ones. In this latter connection, the ideal of course would be to treat the contact who was responsible in the first instance—if he can be found—and to insist on his wearing a contraceptive sheath during intercourse till all warts have been destroyed.

Incarcerated haemorrhoid with warts
LOCAL APPLICATIONS
The following medicines can be applied to the affected area (topical treatment) at home:
Imiquimod (such as Aldara)
Podofilox lotion or gel (such as Condylox)
Sinecatechins (such as Veregen)
The agent that has been most widely used for this purpose is the cytotoxic preparation podophyllin which was introduced for this purpose in 1942. Podophyllin is intensely irritating; it is usually applied once in the morning and again in the evening for 3 days followed by a 4 day rest period. If the warts do not go away, then this cycle is repeated up to 4 times. The method of application is to paint the fluid accurately on the warts with the aid of a stick mounted with a cotton-wool bud, avoiding the perianal skin as far as possible. To this latter end also the buttocks are kept separated so that the skin does not come into contact with the podophyllin on the warts. After five to ten minutes the excess fluid is dabbed off and a talc dusting powder is applied to the surrounding skin. Authors have reported that the average number of treatments needed in their series was four. Twenty-five per cent of their patients developed recurrences, which were usually treated by repeat short courses of bichloracetic acid.
SURGICAL DESTRUCTION OR REMOVAL
Diathermy Excision and Coagulation
This technique has till recently been the classic method of surgical treatment. If the warts are not too extensive and if the patient is fully co-operative, it can be performed without a general anaesthetic and with the aid solely of an infiltration of local analgesic. If the patient is unduly apprehensive, a short sedo-anaesthetic is preferable. The individual warts are then dealt with in turn, either by diathermy coagulation if small, or by diathermy excision or a mixture of excision and coagulation if larger. The practice of using diathermy seems to have been prompted mainly by the hope that it would control bleeding . Unfortunately it is very difficult with it to avoid quite widespread destruction of skin if the warts are extensive. The result is a large wound area, much of which has to heal by granulation, making removal of anal warts by this technique one of the most painful of minor rectal operations. The period required for complete healing may be prolonged and, if the granulating area in the perianal region or anal canal should be circumferential, a fibrous stenosis may develop. During the operation special care should be taken in every case to ensure that all warts in the anal canal itself have been dealt with.
Cryotherapy
With the introduction of cryotherapy it was natural to consider the use of this method for the destruction of anal warts. It has the advantage over diathermy coagulation that the actual freezing process is painless (though the subsequent necrosis and separation of sloughs may be quite painful). In other words, it is often possible to carry out the treatment without anaesthesia provided that adequate access can be obtained to the anal canal to treat any warts within it. As for the technique of freezing, the same sort of cryoprobe with nitrous oxide or liquid nitrogen circulating through it is used as for destruction of skin laesions.
Surgical Excision
In excising anal warts, Thomson and Grace (1978) have stressed the importance of removing just the warts themselves whilst conserving all the intervening skin in order to keep the resulting raw areas as small as possible to prevent excessive discomfort and scarring. For that reason they do not use diathermy but rely entirely on minimal excision with fine scissors. The operation is most conveniently done under general anaesthesia. A very useful initial step is to infiltrate the subcutaneous tissues of the affected anal and perianal regions with a generous amount of a weak solution of adrenaline to stretch the skin and separate the warts, and also to help with haemostasis. Each wart is then lifted up with forceps and snipped off with fine scissors, conserving all normal skin between lesions. If necessary, diathermy may be lightly applied to the raw areas for haemostasis, but it is better to rely mainly for this purpose on pressure with gauze soaked in a topical adrenaline solution. A special search should be made with a bivalve speculum foe any warts lying in the anal canal . Finally, a Milton or adrenaline gauze dressing is applied. The after-care follows conventional
IMMUNOTHERAPY
Immunotherapy for the treatment of cutaneous warts, including some condylomata acuminata was first practised by Biberstein (1944) with very good results, but did not attract much attention till the reports of Powell et at. (1970) and Neland Fourie (i973), who also had high rates of success with it. But the greatest experience with this method of treatment has been that of Abcarian of Chicago (Abcarian et al. 1976; Abcarian and Sharon 1982).
The principle of the treatment is that an autogenous vaccine is prepared from some of the wart tissue that has been excised from the patient and is then administered to him by injection
Collection of Condyloma Tissue.
Tissue for preparation of the vaccine is obtained by excising: some of the warts under general or local anaesthesia without necessarily attempting a complete clearance of them.
Preparation of Cell Cultures and Vaccine. For details of the laboratory technique for preparing: the vaccine, Abcarian et al. (1976) should be consulted.
Vaccination of Patients.
The vaccine is stored in a frozen state. Each week for six weeks 0.5 ml of kis injected subcutaneously. Results. What makes Abcarian’s experience so valuable is that he has maintained a very close follow-up on his patients treated by immunotherapy and in his latest publication records the results in 200 cases followed up front one to eight years with a mean of 46 months.
CONCLUSION REGARDING CHOICE OF TREATMENT
Beyond a shadow of doubt the most effective treatment available for anal warts appears to be immunotherapy with an autogenous vaccine, which is apparently capable of achieving a lasting cure in the great majority of cases. The main objection to this form of treatment is that it requires laboratory support to prepare the vaccine, and it is for that reason that other more easily applied treatments continue to be the ones chiefly employed for this condition, despite their frequent failures. In Britain the usual plan of management is to try podophyllin in the first instance, repeating the course for any recurrences for a while, and reserving surgical measures for initial failures or persistent recur¬rences.
MALIGNANT CHANGE IN CONDYLOMATA ACUMINATA
Though rare, malignant degeneration of anal warts can occur, as has been reported by a number of authors. This development calls for biopsy diagnosis and appropriate radical surgical treatment if feasible
GIANT CONDYLOMA ACUMINATA
What amounts to a malignant condition without being an actual carcinoma is that known as a giant condyloma. Clinically it appears to be a rapidly growing fungating squamous cell carcinoma which enlarges rapidly and spreads widely, histological examination shows no evidence of invasive tumour. The growth causes extensive destruction of adjacent structures by pressure necrosis, which in a lesion of the anal and perineal region means the tissues of the perineum, ischiorectal fossae and even the anorectum itself.
Treatment by irradiation has not proved effective and the best prospect of cure apparently lies with radical surgical excision at an early stage of the condition.